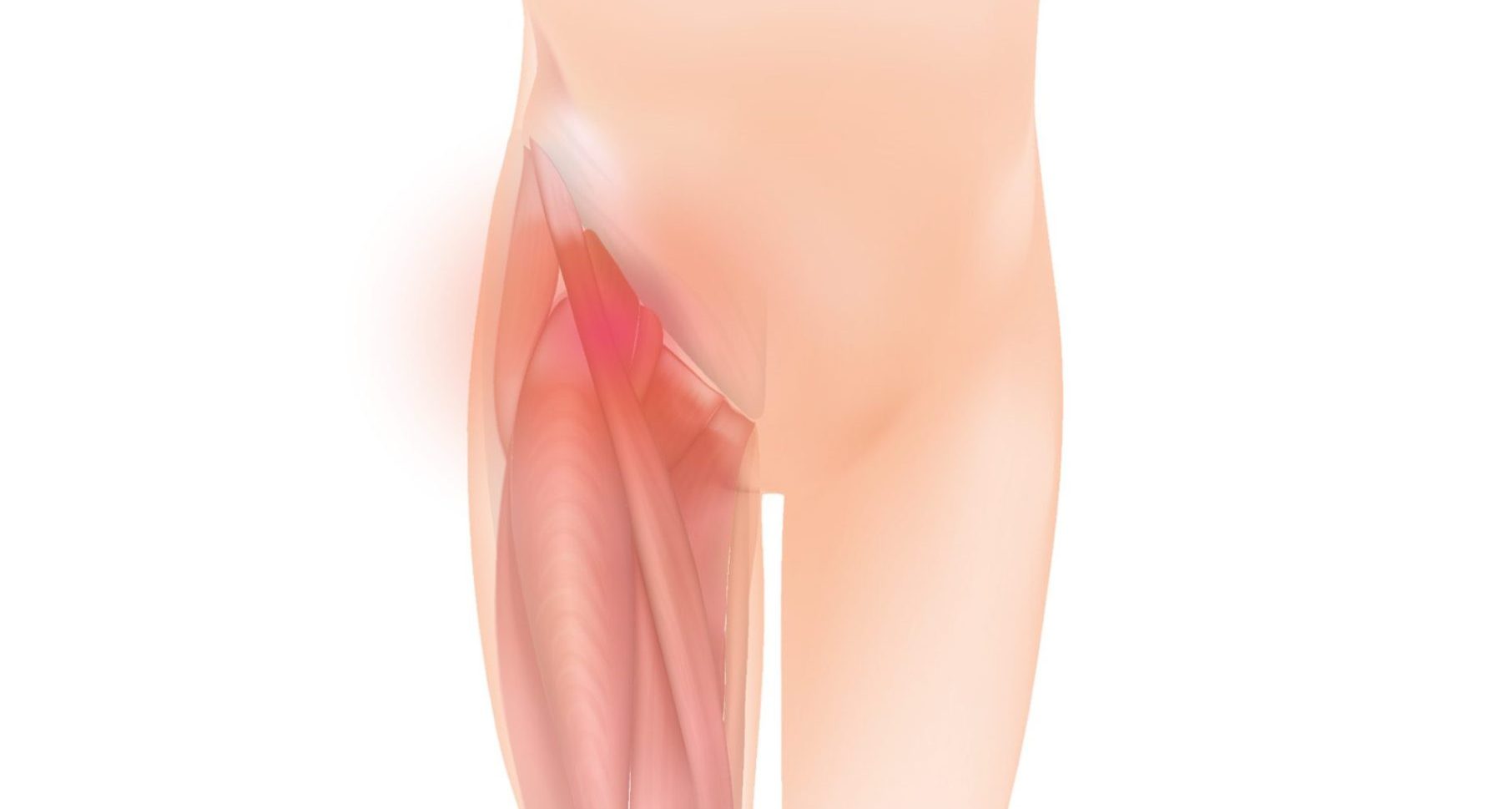
Hip dysplasia is a condition characterized by abnormal development or alignment of the hip joint. It can affect people of all ages, from infants to adults. In hip dysplasia, the hip socket may be shallow or poorly formed, causing instability and potential joint dislocation. The condition can lead to various symptoms and functional limitations.
Symptoms of hip dysplasia may vary depending on the severity of the condition. Infants and young children may exhibit signs such as limited range of motion, uneven leg lengths, clicking or popping sounds in the hip joint, or a leg that turns outward. In adults, hip dysplasia can cause hip pain, stiffness, difficulty walking, and increased susceptibility to hip joint injuries such as labral tears or osteoarthritis.
The management of hip dysplasia often involves a multidisciplinary approach, with physiotherapy playing a crucial role in the treatment and rehabilitation process.
Applying the 5 stages of rehab can help address the specific needs and challenges associated with hip dysplasia.
Pain and symptom management: The initial stage of rehab focuses on managing pain and reducing inflammation. Pain-relieving medications may be prescribed by a healthcare professional. Physiotherapy treatments such as heat or cold therapy, muscle activation exercises and gentle mobilization techniques can help alleviate pain and promote healing.
Range of motion: Once pain is under control, the focus shifts to improving the range of motion in the hip joint. Physiotherapy exercises and stretches are prescribed to enhance hip flexibility and increase the joint’s mobility. This may include gentle hip movements in different planes, such as flexion, extension, abduction, adduction, and rotation, that are gradually progressed as tolerated.
Motor control: In stage 3, the emphasis is on improving neuromuscular control and stability around the hip joint. Specific exercises are prescribed to target the muscles surrounding the hip, including the hip stabilizers, glutes, hip abductors, and hip external rotators. Strengthening these muscles helps provide support and stability to the hip joint, reducing the risk of instability or dislocation.
Strengthening: Stage 4 focuses on strengthening the muscles around the hip joint to enhance joint stability and function. Exercises that target the hip and core muscles, such as squats, lunges, bridges, and clamshells, are incorporated into the rehab program. Strengthening exercises should be performed with proper form and progression to gradually build strength and endurance.
Maintenance: The final stage of rehab involves maintaining the gains achieved in the previous stages and preventing future hip problems. This may include a customized exercise program that includes strength training, flexibility exercises, and functional activities. It is important to continue with regular exercise and maintain good hip mechanics during daily activities and sports participation to support long-term hip health.
Throughout the rehab process, close collaboration with a physiotherapist or healthcare professional is crucial. They will assess the individual’s specific needs, monitor progress, and make necessary modifications to the rehab program. Additionally, in some cases, surgical intervention may be required to correct the structural abnormalities associated with hip dysplasia. In such cases, post-operative physiotherapy plays a vital role in rehabilitation and optimizing outcomes.
By following a comprehensive and personalized rehab program, individuals with hip dysplasia can experience reduced pain, and improvement in joint function and overall quality of life.
For further information regarding hip dysplasia please visit:
https://www.healthdirect.gov.au/hip-dysplasia
https://www.rch.org.au/kidsinfo/fact_sheets/Developmental_dysplasia_of_the_hip_DDH/
https://www.physio-pedia.com/Hip_Dysplasia